Breast density notification randomised controlled trial at BreastScreen Queensland Sunshine Coast and Brisbane Northside Services: Information for Health Professionals
Research objectives
BreastScreen Queensland Sunshine Coast and Brisbane Northside Services are conducting a randomised controlled trial to assess the effect of notifying women participating in population-based breast screening of their breast density on their psychosocial outcomes and health services use, and to determine whether using different modes (written vs online) of communicating this information alters these effects.
What the study involves
This randomised-controlled trial includes 3 arms that will compare amongst women with dense breasts determined from the mammogram:
- standard care in BreastScreen Australia (no notification of breast density); vs.
- notification of breast density plus a hard-copy written health literacy sensitive information insert; vs.
- notification of breast density plus a link to an online video-based health literacy sensitive information (via a page on the BreastScreen Queensland website visible only to study participants).
The additional health literacy sensitive information provided to participants includes a brief explanation of breast density, suggested actions participants could take, and a discussion of the risks and benefits of those actions. The actions include being more ‘breast aware’ and discussing possible additional testing with a General Practitioner (GP). Information to help inform your discussions with patients is below for your reference.
The woman’s nominated GP will be provided with the participants’ mammogram results as per standard BreastScreen Queensland process (that is, only if the woman has provided her GP’s details to BreastScreen Queensland). GPs will also be provided with the breast density results of participants in trial arms 2 and 3 (that is, participants who receive their breast density results). Note for women in Arm 1 who do not receive a breast density notification, as per usual care their respective GP will also not receive the breast density result. For women who don’t have a nominated GP, participants may still discuss their mammogram results including breast density information and the trial with their GP. If needed, these GPs can call BreastScreen Queensland Sunshine Coast or Brisbane Northside Service and request additional information, or may contact the study researchers at The University of Sydney.
Research participants will be asked to take three surveys online as follow-up for outcomes over two years. Each survey will take less than 10 minutes to fill out.
Why the study is important
The findings of this study will show the immediate and long-term impact of breast density notification on women, GPs, and screening services and will help inform future policy and practice decisions on this important issue.
How clients can be referred to the study
To participate in this study, eligible, asymptomatic women aged 40 to 74 years need to book a screening mammogram at a BreastScreen Queensland Sunshine Coast or Brisbane Northside Service location. Sunshine Coast Service locations include Nambour, Caboolture, Caloundra, Gympie, Maroochydore, Noosaville, the Sunshine Coast University Clinic, and various mobile van locations. Brisbane Northside Service locations include Chermside, Keperra, North Lakes, Redcliffe, Indooroopilly, and Brisbane City (David Jones Rose Clinic).
For more information about who is eligible to attend BreastScreen Queensland for a screening mammogram, visit the 'Who can have a breast screen?' page.
Please note that BreastScreen Queensland doesn’t offer diagnostic mammograms for women with breast symptoms or specific breast clinical concerns.
All about breast density
Mammographic breast density is one of several risk factors for breast cancer. Dense breasts are conventionally classified as having predominantly heterogeneously or extremely dense breast tissue on mammography (Category C or D), using the Breast Imaging Reporting and Data System (BI-RADS). Dense breast tissue can obscure a tumour when interpreting a mammogram as both appear white. Therefore, having dense breasts reduces mammographic sensitivity and can increase a screening participant’s chance of being diagnosed with breast cancer between routine screening mammograms (i.e.., interval cancer). It is estimated that 25-50% of the female population of breast screening age (40 to 74 years) in Australia have dense (heterogeneously and extremely dense) breasts. These estimates vary depending on age, as breast density usually decreases with age, and how breast density is measured and classified.
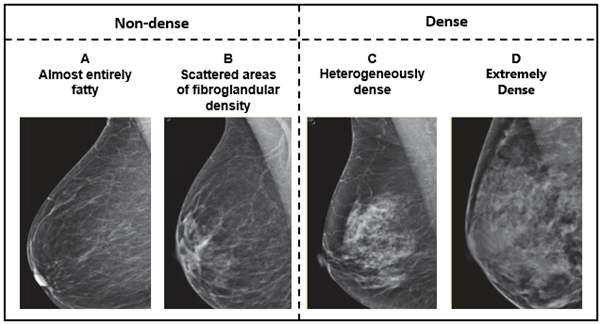
Adapted from American College of Radiology: Breast Density
There is considerable debate and discussion about the potential benefits and harms of routinely measuring and notifying women on a population level about their breast density when they have a mammogram. While notifying women may help them make informed decisions about screening, there is limited evidence on the long-term health outcomes and consequences.
How breast density will be measured in the study
BreastScreen Queensland Sunshine Coast and Brisbane Northside Services will use the fully-automated software, Volpara, to measure breast density. This does not alter the screening test: clients will not be exposed to additional radiation and screening will occur in the same manner as standard care.
BreastScreen Australia's standpoint on breast density
BreastScreen Australia’s position statement recommends against the routine reporting and notification of density within the national screening program. It states that the recommendation will be reviewed when there is an evidence base to inform guidelines and it is supporting research in this area. Individual state screening services have the option to notify their own clients – currently BreastScreen Western Australia and BreastScreen South Australia both do so. Many radiology providers outside the screening program also routinely report breast density in the mammogram report.
What to advise your patients if they have dense breasts
Conversations around breast density are complex. Dense breast tissue is a risk factor for breast cancer. However, there is no consensus on how this risk should be communicated to women or how women should be advised to manage the risk from having dense breasts.
Supplementary screening can be an option for management for some women:
- Supplementary screening – imaging tests (for example, ultrasound or MRI) in addition to mammography – increases cancer detection and can reduce interval cancer rates in women with dense breasts.
- At present, there are no randomised controlled trials with sufficient follow-up to show if supplemental screening saves additional lives in asymptomatic women with dense breasts who have no other risk factors for breast cancer.
- Based on one study of MRI screening (Bakker, 2019) it has been projected that it could have additional benefit for those with extremely dense breasts.
- Supplemental screening can be associated with additional costs, much higher false-positive results than mammography and a higher biopsy rate. In the absence of clear evidence that supplemental testing improves longer term health outcomes, there is also concern that some of the cancers detected with supplemental tests could represent overdiagnosis (diagnosis of clinically non-progressive cancers).
- Currently, mammograms remain the only universally recommended screening test for all women (in all density categories).
Shared decision-making between women and GPs is essential for informed decision on best management. When deciding on supplemental screening, breast density should be taken into consideration with other risk factors (for example, strong family history).
Pathways for a patient who wants to get supplemental screening
Women who are seeking supplemental screening can be referred for breast imaging or a breast specialist opinion, but there may be financial implications. Private radiological services will accept referrals for supplemental screening investigations such as breast ultrasound and breast MRI. However, there is no Medicare rebate available for women with a low risk if they choose these screening options within the private sector. Women with a very high-risk family history may be eligible to have a private breast MRI with Medicare rebate or performed publicly through the SCUH Medical Imaging Department. Supplemental breast ultrasound screening may be available through the SCUH Medical Imaging Department. However, please note that the Royal Brisbane Women’s Hospital will not accept referral for supplemental screening at this time. You can also contact a nurse from BreastScreen Queensland Sunshine Coast or Brisbane Northside Service for additional information about referral pathways for women with dense breasts.
Who to contact to learn more about the study
BreastScreen Queensland is conducting this study in partnership with researchers and clinicians at The University of Sydney. The trial is being funded by the National Health and Medical Research Council and the National Breast Cancer Foundation.
For more information, please contact:
Dr Brooke Nickel 02 9351 7829 or breastdensity.study@sydney.edu.au
BreastScreen Queensland Sunshine Coast Service: 07 5470 5037
BreastScreen Queensland Brisbane Northside Service: 07 3350 7444
Useful links
Clinical Oncology Society of Australia: Mammographic / Breast Density: Facts and Issues
BreastScreen Australia: Position statement on breast density and screening
BreastScreen Queensland: Who can have a breast screen?
BreastScreen Queensland: Information for health professionals
Medicare Criteria for a Bulk Billed Specialist Referred Breast MRI: Item 63464 | Medicare Benefits Schedule
Reference
Bakker MF, de Lange SV, Pijnappel RM, Mann RM, Peeters PHM, Monninkhof EM, et al. Supplemental MRI Screening for Women with Extremely Dense Breast Tissue. N Engl J Med. 2019;381(22):2091-102.
Last updated: March 2024